Maternal Suicide Resource Center
Congressional Briefing
Congressional Briefing on Maternal Suicide
The Congressional Briefing on Maternal Suicide, moderated by Benjamin Miller of the Policy Center for Maternal Mental Health, highlighted the urgent need for action due to its status as a leading cause of maternal mortality.
Policy Recommendations Include:
Congress:
➡️ Expand funding for state Maternal Mortality Review Committees (MMRCs) and Perinatal Quality Committees (PQCs) to implement the Zero Suicide Framework
➡️ Create a Federal Maternal Psychiatry Consultation Program to permanently fund existing state programs and expand to other states (HRSA)
➡️ Revise Child Welfare Law (CAPTA) to Remove Mandatory Reporting to
➡️ Child Protective Services in favor of Safety Plans when a Patient is suicidal
Ensure all women have Access to Maternity Care via Infrastructure (like libraries, roads, police, etc.)
Centers for Medicaid and Medicare Services (CMS):
➡️ Require states to report the HEDIS Perinatal Depression Screening Measures
➡️ Require measures for suicide screening/assessment and safety plan development in primary care and obstetric settings
Click on an infographic to view larger and download the image to share on social media.
Recommended Citation:
Policy Center for Maternal Mental Health. (2023, September). Maternal Suicide in the U.S.: Opportunities for Improved Data Collection and Health Care System Change [Issue Brief]. https://www.policycentermmh.org/issue-briefs-and-papers
Maternal Suicide Awareness Month
Key Dates:
September
Suicide Awareness and Prevention Month and Maternal Suicide Awareness Month
Maternal Suicide Awareness Week
Annually, Maternal Suicide Awareness Week happens during the week of World Suicide Prevention Day, which takes place on September 10th each year.
In 2024, Maternal Suicide Awareness Week will take place from September 9-13, 2024. Use this zoom background throughout the month of September to raise awareness and show your support during virtual meetings.
History of Maternal Suicide Awareness Week and Remembrance Vigil
- Then, research suggested suicide was a leading cause of maternal mortality; however, data on U.S. maternal suicide was not available. Our ultimate goal was to drive action in improving the reporting of maternal suicide rates in the U.S. and implementing programs to prevent maternal suicide.
- During this time, we hosted webinars, provided fact sheets and social media toolkits and posts, and hosted the remembrance candlelight vigil with families impacted by maternal suicide to say the names of mothers lost.
- Though the Policy Center no longer produces a social media toolkit annually, the Policy Center posts may be shared on social media, and/or facts can be pulled from our maternal suicide reference materials.
Facts About Maternal Suicide
CDC Report on Pregnancy-Related Deaths: Data from Maternal Mortality Review Committees in 36 US States, 2017–2019
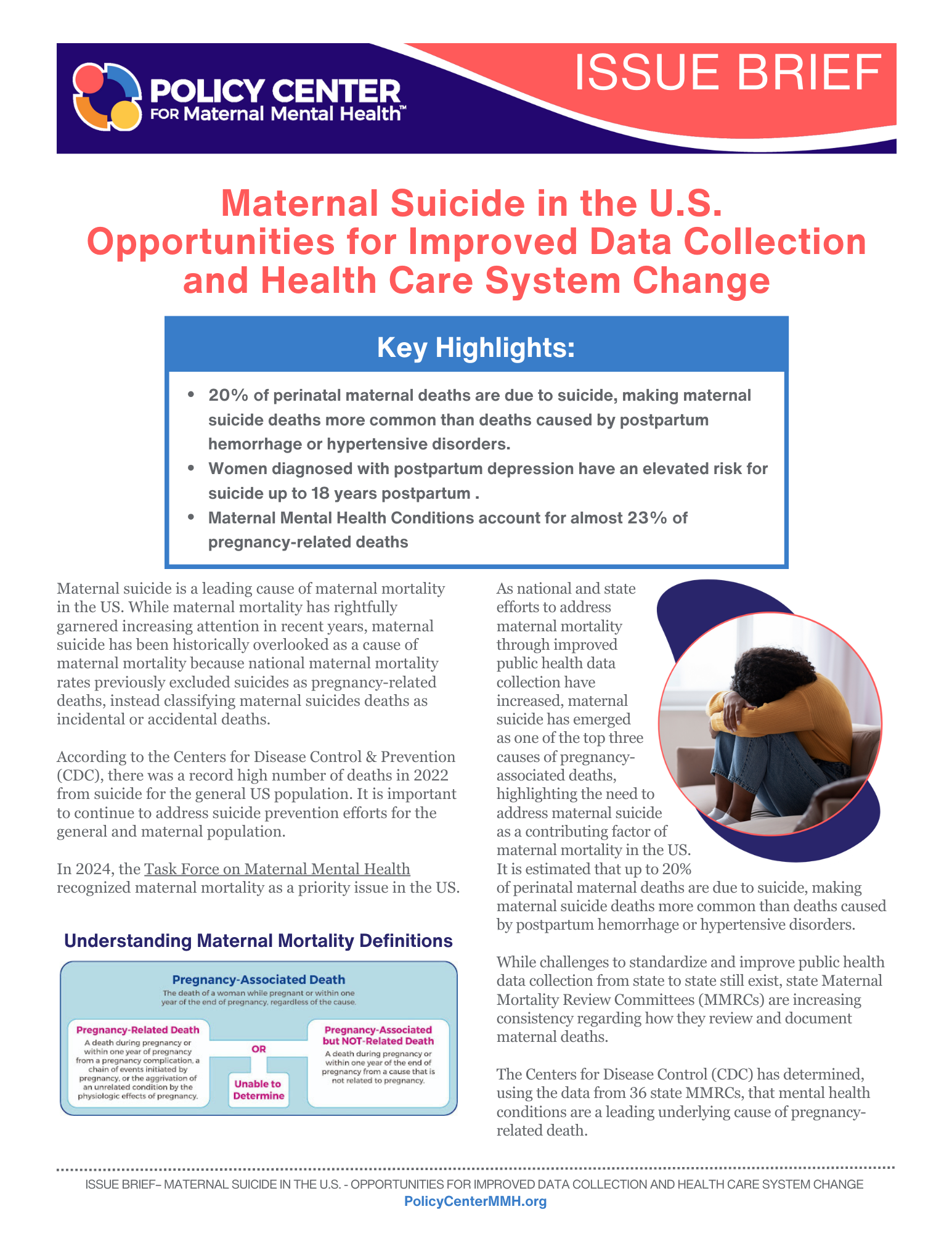
In September 2022, the CDC released a report on maternal mortality. Mental health conditions (including deaths by suicide and overdose/poisoning related to substance use disorder) were the leading underlying causes of pregnancy-related death, accounting for 23% of the deaths. More than 80% of pregnancy-related deaths were preventable.
The following are resources for those working to advance maternal suicide prevention and support.
Facts About Maternal Suicide
Past Maternal Suicide Webinars
The Latest in Maternal Suicide Trends Fireside Chat

Join the Policy Center for Maternal Mental Health leaders to discuss the latest trends in maternal suicide, as noted in the re-released issue brief titled Maternal Suicide in the U.S.
Facts About Maternal Suicide
Maternal Suicide in the U.S., The Latest Research & Data Collection Efforts 2022

Maternal suicide is a leading cause of maternal mortality. With efforts made by the policy organization, 2020 Mom, and the CDC, the U.S. has made significant progress on tracking and reporting maternal suicide rates. However the work to identify maternal suicides is left to the states through reviews conducted in Maternal Mortality Review Committee (MMRC) settings. Additionally, state-based Perinatal Quality Collaboratives (PQCs) are generally charged with facilitating change based on MMRC findings.
This webinar covers:
- A general overview of maternal suicide statistics in the US
- Updated data from the CDC on Maternal Mortality Review Committees and pregnancy-related suicide deaths.
- How states are improving suicide detection in their MMRC process, including the role of informant interviews in identifying maternal suicide deaths, a process adopted by the Delaware MMRC and others
- 2020 Mom’s latest issue brief – suicide tracking and prevention
- Colorado’s latest report illustrates suicide is the top cause of maternal death, and efforts the PQC is championing
- Challenges and opportunities
Facts About Maternal Suicide
Maternal Suicide in the U.S., The Latest Research & Data Collection Efforts
Maternal suicide is a leading cause of maternal mortality. Despite common misconceptions, pregnancy and the postpartum period do not protect against the risk of psychiatric disorders or suicide. It has become increasingly urgent and important to normalize the discussion of maternal suicide to raise awareness and double-down on maternal suicide tracking and prevention efforts. In this webinar, we will cover:

- A general overview of maternal suicide research and data collection in the U.S.
- The difference between suicide risk and suicidal ideation, including racial disparities
- Maternal suicide risk factors
- Efforts to Standardize Review by Maternal Mortality Review Committees
Facts About Maternal Suicide

Sidra Goldman-Mellor, Ph.D., M.P.H.
Lead Investigator, Maternal drug-related death and suicide are leading causes of post-partum death in California
Associate Professor of Public Health
School of Social Sciences, Humanities, and Arts
Director, HSRI Biostatistics and Data Support
University of California, Merced

Marcela Smid, MD MA MS
Lead Investigator: Pregnancy-Associated Death in Utah: Contribution of Drug-Induced Deaths
Assistant Professor, Division of Maternal Fetal Medicine
Department of Obstetrics and Gynecology
University of Utah
Medical Director of SUPeRAD (Substance Use and Pregnancy – Recovery, Addiction, Dependence) Clinic

Kara Zivin, PhD, MS, MA, MFA
Researcher and Peer with Lived Maternal Mental Health Experience
Lead Investigator, Trends in Suicidal Ideation and Self-Harm Among Privately Insured Delivering Women
Professor of Psychiatry, Obstetrics and Gynecology, Health Management and Policy/Public Health
University of Michigan
Faculty Associate, Survey Research Center
Institute for Social Research
Research Career Scientist, Center for Clinical Management Research (CCMR),
VA Ann Arbor Healthcare System
Facts About Maternal Suicide
2020 Mom & Zero Suicide Institute Webinar – The National Zero Suicide Initiative: Levers for Maternal Mental Health

2020 Mom and our partner, Zero Suicide Institute, learned and discussed the national Zero Suicide framework, a system-wide, organizational commitment to safer suicide care in health and behavioral health care systems.
The framework is based on the realization that suicidal individuals often fall through the cracks in a sometimes fragmented and distracted health care system. A systematic approach to quality improvement in these settings is both available and necessary.
Inspired by health care systems that had seen dramatic reductions in patient suicide, the Zero Suicide began as a key concept of the 2012 National Strategy for Suicide Prevention and quickly became a priority of the National Action Alliance for Suicide Prevention (Action Alliance), and a project of Education Development Center’s Suicide Prevention Resource Center (SPRC), supported by the Substance Abuse and Mental Health Services Administration (SAMHSA).
The U.S. health delivery system was already struggling to effectively address and prevent suicide, now with pandemic stressors expected to increase suicide rates, health systems can take action by adopting the Zero Suicide framework and tools.
Moderator:
Joy Burkhard, MBA
Executive Director, 2020 Mom
Panelists:
Julie Goldstein
Director, Zero Suicide Institute
Edwin Boudreaux, PhD
Professor, Departments of Emergency Medicine, Psychiatry, and Population and Quantitative Health Sciences
University of Massachusetts Medical School
Facts About Maternal Suicide
Maternal Suicide: What All Providers and Advocates Should Know

Presenters:
SUSANNA TROST, MPH
Maternal Suicide Stats
CDC Maternal Mortality Prevention Team, Division of Reproductive Health
JENNIFER BEAUREGARD, PhD
CDC Maternal Mortality Prevention Team, Division of Reproductive Health
MARY CLAIRE KIMMEL, MD
Maternal Mental Health
Suicide Nuances
Assistant Professor, Department of Psychiatry at University of North Carolina at Chapel Hill
KAREN TABB DINA, PhD
Differences in Maternal Suicidal
Thoughts in BIPOC Community
University of Illinois at Urbana-Champaign
RACHAEL KENTER, MPH, CHES
Upstream Prevention
& Zero Suicide Initiative
Suicide Prevention Resource Center
SHYE LOUIS, M.Ed.
Crisis Prevention
National Suicide Prevention Lifeline
In this webinar, we covered the latest on suicide prevention and facts about maternal suicide, including:
- A general overview of suicide and COVID related increases
- Maternal mental health statistics including maternal suicide
- General crisis prevention efforts
- Suicide prevention efforts
Facts About Maternal Suicide
Suicide Prevention Resources
- The American Foundation for Suicide Prevention has resources to assist with setting and communicating policy priorities on suicide prevention, as well as infographics to share.
- Read about CDC’s suicide prevention strategic plan, grounded in data, science, action, and collaboration.
- Explore CDC’s Preventing Suicide: A Technical Package of Policies, Programs, and Practices for strategies and approaches with the best available evidence to prevent suicide.
- The Zero Suicide Toolkit: a detailed guide to Zero Suicide implementation and strategy.
- The Collaborative Assessment and Management of Suicidality (CAMS): a flexible therapeutic framework in which patient and provider work together to assess the patient’s suicidal risk and use that information to plan and manage suicide-specific, “driver-oriented” treatment. It is a philosophy of clinical care that can be used for a wide range of suicidal patients across outpatient and inpatient treatment settings and in the context of various psychotherapies and treatment modalities.
- Care Transitions Outpatient Health Care Self-Assessment from National Action Alliance for Suicide Prevention
- The Outpatient Self-Assessment is a checklist designed to help outpatient behavioral health care systems assess their policies, procedures, and practices as they compare to the Best Practices in Care Transitions for Individuals with Suicide Risk: Inpatient Care to Outpatient Care. The results of the self-assessment will help outpatient health care systems identify opportunities to improve administrative practices and clinical care.
- Outpatient Care Transitions Action Planning template from National Action Alliance for Suicide Prevention. The Outpatient Action Planning template was developed to translate the results of the self-assessment into action steps that will incrementally improve their overall care transitions and patient care practices.
- Suicide Safety Plan: A safety plan app that allows you to customize your own warning signs that a crisis may be developing, coping strategies for dealing with suicidal urges, places for distraction, friends and family members you can reach out to, professionals you can call, methods of making your environment safe, and your own important reasons for living.
In this webinar, we covered the latest on suicide prevention and facts about maternal suicide, including:
- A general overview of suicide and COVID related increases
- Maternal mental health statistics including maternal suicide
- General crisis prevention efforts
- Suicide prevention efforts
Facts About Maternal Suicide
Guide on Suicide and Serious Mental Illness
People who live with serious mental illness (SMI)—such as major depression, bipolar disorder, and schizophrenia—are at increased risk of suicide. It is critical to understand the problem of suicide for those who have SMI. That is the only way to create a comprehensive, effective suicide prevention plan.
SMI Adviser and the Suicide Prevention Resource Center (SPRC) are proud to present a new guide on Suicide and Serious Mental Illness. It is an ideal resource for both suicide prevention coordinators and mental health clinicians.

Facts About Maternal Suicide
Why Screen for Maternal Suicide Risk?
Screening Tools
Several suicide screening tools exist; the Columbia Suicide Severity Rating Scale (C-SSRS) is robust in assessing for ideation and risk.
The Columbia-Suicide Severity Rating Scale (C-SSRS) is a tool that can be used in many settings, including, community settings, medical, inpatient, and outpatient behavioral health.
The C-SSRS assesses the full range of evidence-based ideation and behavior. It can be used as an initial screener or as part of a full assessment.
Those who administer the screening for maternal mental health disorders may wish to use the C-SSRS if a person verbally discloses suicidal thoughts or answers “yes” to question 9 on the PHQ-9 or question 10 on the EPDS, for example.
Additionally, the SAFE-T Suicide Assessment Five-Step Evaluation and Triage may be utilized to understand both access to potential deadly tools and protective factors.
Download the C-SSRS or combined C-SSRS & SAFE-T tools here:


Or you can create your own screening toolbox by visiting the Columbia C-SSRS Lighthouse Project’s website.
Free Training
Though training is not required to administer the screener, it can be helpful. Training provides an overview of the C-SSRS instrument and teaches how and when to administer it in real-world settings
Watch a Pre-Recorded Webinar
Watch a webinar on your own schedule by going to the Columbia University C-SSRS Light House Project’s YouTube channel and selecting an archived webinar. They are available in 30 languages and are less than an hour long.
Facts About Maternal Suicide
Monitoring Federal and State Maternal Suicide Reporting Efforts
The blog posts below share our analyses of how the U.S. is progressing in its journey to report a national maternal suicide rate. Follow our blog by signing up for 2020 Mom’s enews to keep abreast of the slow but steady efforts and progress being made.