On April 17, the American College of Obstetricians and Gynecologists (ACOG) released a new consensus statement titled “Tailored Prenatal Care Delivery for Pregnant Individuals.” It was endorsed by the American College of Nurse-Midwives; the Association of Physician Associates in Obstetrics and Gynecology; the Association of Women’s Health, Obstetrics and Neonatal Nurses; the National Association of Nurse Practitioners in Women’s Health; and the Society for Maternal-Fetal Medicine.
The consensus statement acknowledges that the current prenatal care paradigm was developed nearly 100 years ago in 1930, and it is time to reevaluate prenatal care delivery standards. The statement includes three changes: 1.screening for social drivers of health (SDoH), 2. adjusting the number of prenatal care visits based on patient risk/need, and 3. incorporation of telehealth.
More specifically, the statement calls for a potential reduction in the number of routine visits (currently 12 to 14 in-person visits) to fewer for healthy pregnancies, and potentially more for those with higher risk pregnancies (noting however, “a change in the delivery of antenatal care is not warranted for all patients or all clinical situations”) and addresses telehealth; that certain prenatal visits could be telehealth visits when appropriate. The statement calls for clinicians to screen patients for social drivers of health before 10 weeks of pregnancy, coordinating health and community assistance for individuals with unmet needs.
Regarding adjustments to the number of visits for a patient, the consensus states:
“Potential care adjustments include 1) tailored visit schedules (vs traditional) streamlined around needed education and services; 2) telemedicine (vs in-person care) where possible to reduce travel burden, need for childcare, or time away from work; and 3) group prenatal care (vs individual care, ideally in the individual’s native language) to address social isolation and low health literacy.”
The statement emphasizes that visit schedules can and should be adjusted based on clinical needs and personal preferences. For a patient with a low-risk pregnancy and reliable access to virtual care, fewer visits may be completely appropriate—especially if those visits are more comprehensive and person-centered.
Further, the consensus emphasizes shared decision making, where the patient is an informed partner in care planning, including:
- Talking through care options like telemedicine, in-person, or group visits
- Tailoring visit schedules based on what’s most appropriate for the patient’s needs
- Practicing cultural humility and trauma-informed care
Our Response:
We believe it’s critical to routinely reevaluate standards and recommendations to account for new research findings and practice modalities like telehealth. We applaud ACOG for taking this step and urge the Centers for Medicare Services (CMS) and/or State Medicaid Agencies (SMAs) and commercial payors to recognize and address these changes in payment protocol. This should include exploring the value of unbundling services so frequency of appointments and the type of services being provided can be measured and monitored through claims data.
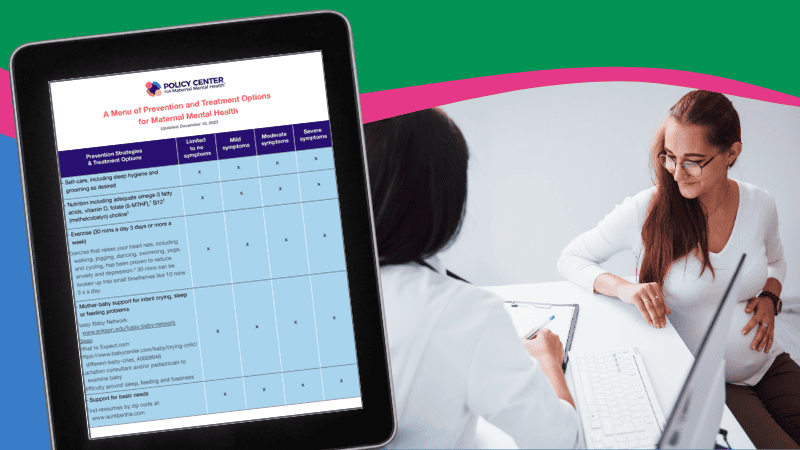
These guidelines do not have a direct impact on maternal mental health as the recommended timeframes for screening (and treatment as needed) are still applicable:
- Obtain individual/family mental health history at intake
- Screen for depression and anxiety at the initial prenatal visit, later in pregnancy, and at postpartum visits
We encourage ACOG to address postpartum visit frequency in more detail by updating its 2018 “Optimizing Postpartum Care” committee opinion, particularly in light of states extending pregnancy Medicaid through 12 months postpartum.
We also hope that additional remote patient monitoring technologies will be incorporated into future perinatal consensus statements and/or that OBs will not be prohibited from utilizing (and being reimbursed for utilizing) remote monitoring technologies, including those that could detect signs of anxiety and depression through monitoring heart rate and changes in sleep patterns, for example.
Let us know your thoughts about the new prenatal care guidelines by emailing [email protected].