The first set of U.S. maternal depression screening data is now available – through HEDIS. Not surprisingly, screening in both pregnancy and the postpartum period was reported at less than 20%.
About HEDIS
The Healthcare Effectiveness Data and Information Set® (HEDIS®) is a national measurement set that assesses how well Medicare, Medicaid, and commercial health insurance plans manage the care of their enrolled populations.
The Prenatal Depression Screening and Follow-Up measure and the Postpartum Depression Screening and Follow-Up measure were released through HEDIS in 2019. Read more here.
This is the first year data is being reported.
These measures assess how often patients covered by commercial (private) insurance plans and Medicaid plans are being screened for depression and how often those who screen positive receive follow-up care. These measures are based on screening guidelines and recommended care from bodies like the US Preventive Services Task Force and the American College of Obstetrics and Gynecology.
The postpartum screening and follow-up measure data are collected by health insurers/plans via electronic data capture systems, not just medical records or claims data, as HEDIS measures were limited to in the past. This means screening from any type of provider (OB, Midwife, Pediatrician) as well as non-providers, like insurance company high-risk pregnancy case managers, could be counted.
The measures require:
- Use of a standardized tool for screening
- Those who screen positive receive some form of proper follow-up.
This can include actions such as a case management encounter, a behavioral health encounter, or medication.
First Set of National Maternal Depression Rates:
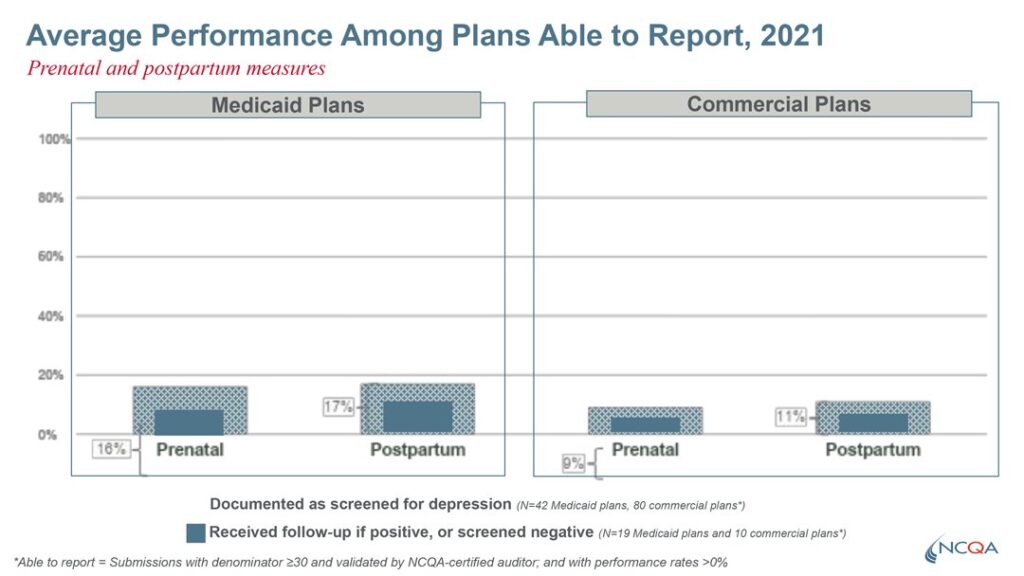
The light blue bar represents patients who were screened. The dark blue bars represent the percentage of mothers who received some type of positive screening and also received some type of follow-up care OR had screened negative. This means that the dark bar represents mothers who presumably received appropriate follow-up care based on their screening.
Less than 20% of patients were screened
The Medicaid Screening and follow rates were 16% during pregnancy and 17% in the postpartum period. For private insurers, screening rates were lower, at 9% during pregnancy and 11% in the postpartum.
A 2019 research review found nearly 50% of women with postpartum depression go undiagnosed, and another recent review observed that only 22% of women screening positive for depression received mental health treatment.
Notably, the HEDIS screening measures included components for both screening and follow-up.
Only half of the patients who screened positive received follow up
As Lindsey Roth from the National Committee for Quality Assurance (NCQA), the organization that develops HEDIS measures, reported on a webinar hosted by 2020 Mom, it is important to point out that this data represents average performance among health plans who were able to access some type of electronic data on these screening measures.
This data was sourced from 50% case management systems, 40% electronic health records, and 10% health information exchanges.
Participation by Plans in Data Collection and Reporting
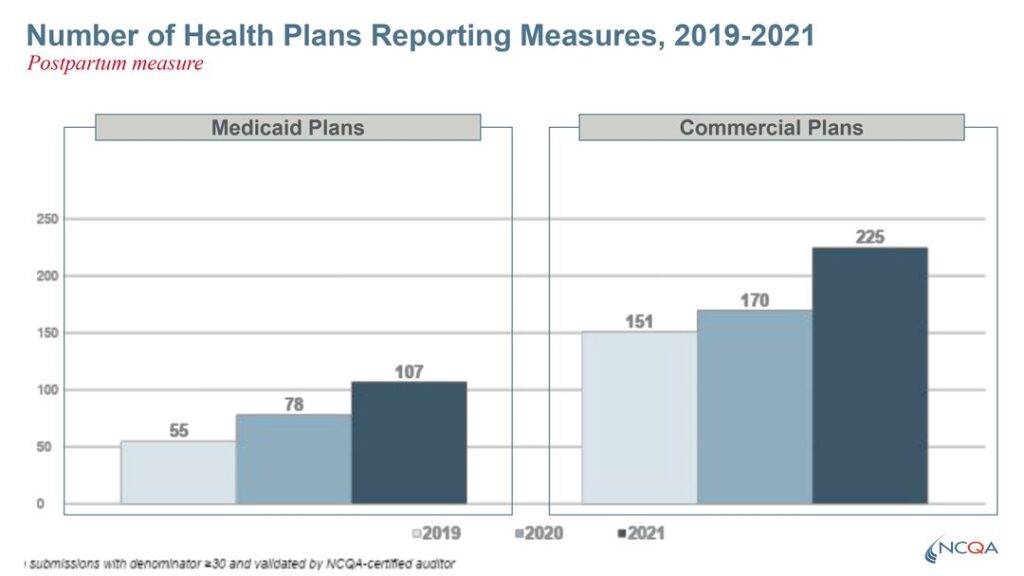
In 2021, 107 Medicaid plans reported the measures, and 225 commercial plans participated in data collection and reporting. This represents approximately half of all Medicaid and Commercial plans that submitted any HEDIS data for any measure that same year.
Conclusion
2020 Mom applauds NCQA for developing the new HEDIS measures, the funders who made the measure development possible, the state Medicaid agencies who are requiring reporting of these measures, and the plans who are collecting and reporting this data.
2020 Mom, with support from our partners, will continue to provide health systems with support and tools to adopt screening protocol, such as:
- Comprehensive screening guidance for providers on validated tools, a sequencing protocol, and screening score cut offs.
- Efforts to expand reimbursement to Obstetricians, the perinatal medical home, for screening and follow-up care.
- Behavioral health workforce support and expansion, including:
- efforts to monitor insurer network adequacy,
- Working with federal bodies on ways to improve the US mental health system through efforts to improve federal mental health parity implementation
- proliferation of state-certified peer support specialists.
Understanding if and when mothers are being screened and treated for maternal mental health disorders is critical data for ensuring mothers get the timely and appropriate care they need.
