Key Highlights
- In a survey of doulas, nearly all shared they have a role to play in educating their clients about maternal mental health disorders, but not in screening given its clinical nature.
- The core competencies for doulas (previously developed by maternal mental health leaders) are being updated to reflect that conducting screening is not a required competency; however, being familiar with screening protocol is.
- Doula training and certification programs should be updated to incorporate the range of maternal mental health disorders and symptoms and align with the updated maternal mental health core competencies for doulas.
Take it To Go
Recommended Citation: Policy Center for Maternal Mental Health. (2025, March). The Role of Birth and Postpartum Doulas in Improving Maternal Mental Health [Report]. http://www.doi.org/10.69764/RBDM2025
Executive Summary
This exploratory research was conducted to understand the role that birth and postpartum doulas (“doulas”) believe they should play in addressing maternal mental health (MMH) and what aspects of maternal mental health are incorporated in current doula training.
We conducted a literature review, surveyed doulas to learn about their practices related to education, screening, and referral for maternal mental health, and conducted a rapid review of current training programs. We compared these findings to the MMH core competencies for doulas developed by the California Task Force on Maternal Mental Health Care in 2017, which was championed by 2020 Mom (now the Policy Center for Maternal Mental Health).1
No national or international training organization appears to be addressing maternal mental health in a manner that aligns with the core competencies. The three community-based doula training organizations that replied to our survey provided responses that illustrate their training is somewhat more aligned with the critical core competencies.
Of the 12 doulas surveyed, nearly all explained that screening was out of scope and that they had a role to play in educating their clients about the risk factors, signs, and types of maternal mental health outcomes. They shared this information through written materials and in conversations with their clients throughout the perinatal period. Some educated their clients’ support partners (partners, close friends, or family members). Doulas often referred clients to mental health resources such as therapists, support groups, and peer support programs throughout the perinatal period. Some educated their clients on the screenings they may be given in their OB’s office. Finally, not surprisingly, some doulas supporting Black clients noted the need to advocate for their clients to buffer the harms of disrespectful care and racism, which have a direct impact on maternal health.
Given these findings, the Policy Center for Maternal Mental Health will be updating the maternal mental health core competencies for doulas to remove references to screening administration. We also recommend that training and certifying organizations align their training with the core competencies and provide continuing maternal mental health training to doulas who have already completed their training or received certification. This training can be provided through existing certification programs for professionals such as doulas.
Introduction
What is a doula?

Birth and postpartum doulas are nonclinical trained professionals who can provide emotional, physical, and informational support during pregnancy, delivery, and after childbirth (to a “client” and their support network).2 While traditional healthcare providers spend 5.75 hours with patients, community-based doulas spend 76 hours (on average) with each client.3 Doula support is linked to a host of improved outcomes, including improved maternal mental health.2 The care doulas provide can include mental health education and resources, connection to community and clinical mental health resources, and emotional support.3 More specifically, the types of services and support doulas provide include:
- Physical support may look like breathing exercises and stretches to help manage labor pain.
- Emotional support may take the form of reassurance, active listening, providing a non-judgemental space, and relieving stress and anxiety.4
- Informational/educational support may include education on the early signs of maternal mental health needs, risk signs for pregnancy complications, lactation education, and skills to effectively communicate their needs to a provider. According to the Prenatal to Three Policy Center, doulas also may teach their clients about “monitoring a fetus’s movements in utero, sleeping patterns, and positions.”5 Doulas may provide information about local resources and help clients access resources to meet material and financial needs.
- Patient self-advocacy may involve helping a client feel empowered and knowledgeable so they can ask a provider if they were screened/can be screened for mental health conditions and helping a client navigate the healthcare system.6 Often, doulas help clients make a birth plan and have more agency over medical decisions surrounding their birth.
Doulas and Maternal Mental Health Training
Doula training is not standardized.7 In addition, existing literature3 shows that doulas vary “in their confidence in identifying perinatal mental health problems.”
Hall et al.8 found that among 252 doulas, an overwhelming majority “desired more training in emotional support” yet only 11% thought it was important for doulas to know when to refer clients to a health provider or community support for mental health needs. Hall et al.8 also found that certification from the DONA International 2017 certification program has “a limited portion” of training dedicated to the “emotional component of the transition to motherhood.” Notably, most of the training components focused on mental health were to be done independently, and were not discussed in detail during in-person training.
Core Competencies: Doulas and Maternal Mental Health
In 2017, the California Task Force on Maternal Mental Health Care, championed by the Policy Center for Maternal Mental Health, developed provider core competencies for maternal mental health.1 The competencies were developed to address the need for baseline knowledge and skills among various provider types, including doulas, in caring for perinatal women.
These core competencies relative to doulas, community health workers, and lactation consultants are:
- Understand signs and symptoms of the range of MMH disorders and which factors place a woman at high risk
- Develop knowledge about valid screening tools for depression and anxiety
- Understand where to locate these screening tools and how to select and use them
- Understand recommended screening frequency during pregnancy and postpartum and suggested ‘cutoff’ scores to identify who may have potential anxiety or depression
- Be familiar with, and follow agency protocols for, different types of healthcare workers involved in addressing MMH, which include prevention and treatment resources and referral pathways
- Understand that trouble breastfeeding can be a risk factor for anxiety and depression, and some agents used to help increase breast milk supply may trigger anxiety
Methods
Our research sought to assess the alignment between the recommended core competencies described above and current implementation in doula education and practice.
Doula Survey
We developed a survey informed by conversations with varying leaders in maternal health about the various roles doulas may or may not fill in providing screening and support relative to maternal mental health care. We distributed the survey through a national listserv for doulas facilitated by NHeLP (National Health Law Program) in November 2024. Responses were received through December 2024. Respondents were asked to answer the following question and provide a brief explanation:
“Are you already, or thinking about, providing MMH support in any of these ways?”
a. Educating clients that MMH disorders, like anxiety and depression, are the most common complications of pregnancy/birth
b. a. + Offering to screen if the client hasn’t been screened recently by her/their OB
c. a + routinely screening and referring to support groups, etc.
d. other?”
Respondents emailed their responses directly to members of the Policy Center for Maternal Mental Health staff. Responses were confidential. We followed up with respondents if we needed clarity or additional detail. As remuneration, participants were offered a complimentary virtual registration to the 2025 Maternal Mental Health FORUM. Twelve (12) doulas responded to our inquiry.
We conducted a type of content analysis called conceptual analysis,9 to quantify response types and reasonings for response types across a wide variety of doula providers. We coded inductively and then compared results to the core competencies.
Doula Training Review
To highlight how the core competencies are present (or not) in doula training, we reviewed the content (e.g., websites, descriptions of training, training content) of doula certification groups for birth/labor and postpartum doula certification. We supplemented our manual search with ChatGPT.10
We reviewed the content of the following international, national, and community-based doula training organization collectives and in comparison to the described core competencies in MMH.11
International Organizations (N=4)
- DONA (Doulas of North America) International12
- Childbirth International13
- International Childbirth Education Association (ICEA)14
- Birth Arts International15
National Organizations (N=1)
- Childbirth and Postpartum Professional Association (CAPPA)16
Local Community-Based Organizations (N=3)
We surveyed community-based organizations in Louisiana, California, New York, Illinois, Washington, Nevada, and Georgia. The survey was anonymous, and three organizations completed it.
The survey clarified the content in their educational materials utilized for certification:
“Are you already, or thinking about, or providing MMH education in any of these ways?”
- Training doulas to understand signs and symptoms of the range of MMH disorders and which factors place a woman at high risk
- Training doulas to develop knowledge about valid screening tools for depression and anxiety
- Educating doulas to understand where to locate these screening tools and how to select and use them
- Educating doulas to understand recommended screening frequency during pregnancy and postpartum and suggested ‘cutoff’ scores to identify who may have potential anxiety or depression
- Helping doulas become familiar with and follow agency protocols for different types of healthcare workers involved in addressing MMH, which include prevention and treatment resources and referral pathways
- Helping doulas understand that trouble breastfeeding can be a risk factor for anxiety and depression, and some agents used to help increase breast milk supply may trigger anxiety
- Other
Do you include education on maternal mental health in your doula training?
- Yes
- No
- Other
What is the format of your MMH education?
- In-person, synchronous
- Virtual, synchronous
- Asynchronous
- Other
Results
Doula Survey Results
A majority of the respondents believed screening, given its clinical nature—and likely because it is the first step in providing a diagnosis—was out of scope. All respondents felt that educating their clients was within their scope of practice when it came to maternal mental health support, and nearly all saw their role as important to refer if/when they noticed or were informed by their clients of symptoms of potential MMH disorders.
Screening
A majority (9/12) of doulas felt that screening was outside their scope of practice because they were not clinical support professionals.
However, several doulas felt they could help ensure patients were screened by informing them that they should expect to receive screening as part of routine practice. One doula shared, “I discuss the Edinburgh (EPDS) scale in my classes and also inquire if their provider (e.g., OB/GYN) has gone over anything similar with them.” noting that this helps clients to not feel afraid or anxious if they encounter something unexpected in the clinic. This respondent went on to share that providers were not giving education on MMH to patients so patients were not aware if/when they were being screened. “The response is generally ‘no,’ or they don’t remember because it was not explained to them – just given as a way to ‘check the box.’”
Educating Clients

Education was often described as improving general knowledge about common mental health conditions, such as anxiety and depression. Doulas shared that many of their clients experience distress and that they help them by identifying what’s “normal” versus what kind of distress suggests they should seek support. Some noted they also share the risk factors for common conditions with their clients. While all respondents said they provided education, three noted that they also educated partners. Other informational support included sharing books and written materials with their clients.
Respondents shared how other supports they provide are integral to the mental well-being of clients. One respondent said, “Lactation support, peer support, advocacy, and resource referrals—none of it can be separated into service silos when a birthing family looks to a doula to help them navigate the healthcare system.” Other respondents shared similar sentiments, such as noticing how sleep is associated with mental health: “[I educate] about and encourage families to create a ‘Protected Sleep Plan.’”
Referral
A majority of doulas (11 of 12) felt that referral to mental health support was a critical part of their role. They saw referrals as important across the perinatal period and not exclusive to the postpartum period or solely the role of postpartum versus birth doulas. For example, one doula commented, “I also highly suggest finding a therapist or counselor before birth just in case.”
Doulas endorse the role of support groups, including those that are both virtual and in-person, therapist-facilitated or held, and virtual support groups without a licensed facilitator. They often referred patients to therapists and support groups. Some doulas worked to address structural barriers to support by ensuring that referrals were both in-person and virtual.
There was variability in the timing of referrals. Some helped their clients identify potential mental health support early in pregnancy in case it was needed. Others focused on the postpartum. One respondent shared, “I screen during postpartum visits and refer them to their provider, mental health providers on my resource list, and support groups. I host a series of postpartum support groups quarterly through my virtual moms support group on social media as well.”
Other doulas waited to refer clients until clients shared mental health concerns or were identified as “high-risk” by the doula, (such as having previously experienced postpartum depression, being pregnant with multiples, or having low social support, for example). In tandem with referrals, some doulas also worked to ensure their clients knew how to navigate the healthcare system. Clients were also supported through additional means (e.g., the National Maternal Mental Health Hotline, Postpartum Support International’s (PSI) Helpline and resources). For example, one doula shared, “I show them the links to call/text PSI and the Maternal Mental Health Hotline for both them or a friend who might be in need. I’ve signed up a few clients for support groups directly with PSI.” Two indicated that they were first aid mental health certified as Peer Support Specialists.
Other Insights
Some respondents offered some additional insights, such as how they strengthen client support systems, support Black clients, and the importance of maintaining their own mental health.
Strengthening Client’s Support System
Two respondents felt that they could support their client’s mental health by strengthening their support system. For instance, one doula shared that she could “empower partners to recognize and do something if they suspect they need more,” educate partners on mental health needs, and connect clients to peer support or support groups.
Supporting Black Clients
There were several doulas who noted that when they were supporting Black clients, their role with mental health looked slightly different. For instance, they advocated for their client to buffer the harms of obstetric racism. In other instances, two worked to provide emotional support following a traumatic birth.
Mental Health of Doulas
Finally, several respondents recognized the importance of the doula’s own mental health and that of their peers—other doulas and community health workers. One respondent said, “The last two years my focus has been reducing the physical health repercussions of toxic stress from persistent racism on Black birth workers who experience secondary trauma on top of their own biased based care as professionals in the field. If the birth workers burn out, what happens to the birthing families?”
Doula Training Review
Following are the results of our data collection regarding doula training.1
| Organization | Training on MMH Signs & Risk Factors2 | Training on Screening Tools & Frequency3 | Referral Protocols for Healthcare Workers4 | MMH & Breastfeeding Challenges5 |
|---|---|---|---|---|
| Birth Arts International (BAI) | ✅ Covers postpartum mood disorders & emotional support | ❌ Not specified | ❌ Not specified | ❌ Not specified |
| ICEA (International Childbirth Education Association) | ✅ Covers postpartum mood disorders & emotional support | ❌ Not specified | ❌ Not specified | ❌ Not specified |
| DONA International | ✅ Covers postpartum mood disorders & emotional support | ❓ No specific information found | ✅ Discusses referrals for support outside scope | ❓ No specific information found |
| Childbirth International | ✅ Covers postpartum mood disorders & emotional support | ❓ No specific information found | ❓ No specific information found | ❓ No specific information found |
2. Corresponds to core competency: Understand signs and symptoms of the range of MMH disorders and which factors place a woman at high risk
3. Corresponds to core competencies: Develop knowledge about valid screening tools for depression and anxiety; Understand where to locate these screening tools and how to select and use them; Understand recommended screening frequency during pregnancy and postpartum and suggested ‘cutoff’ scores to identify who may have potential anxiety or depression
4. Corresponds to core competency: Be familiar with and follow agency protocols for different types of healthcare workers involved in addressing MMH, which include prevention and treatment resources and referral pathways
5. Corresponds to core competency: Understand that trouble breastfeeding can be a risk factor for anxiety and depression, and some agents used to help increase breast milk supply may trigger anxiety
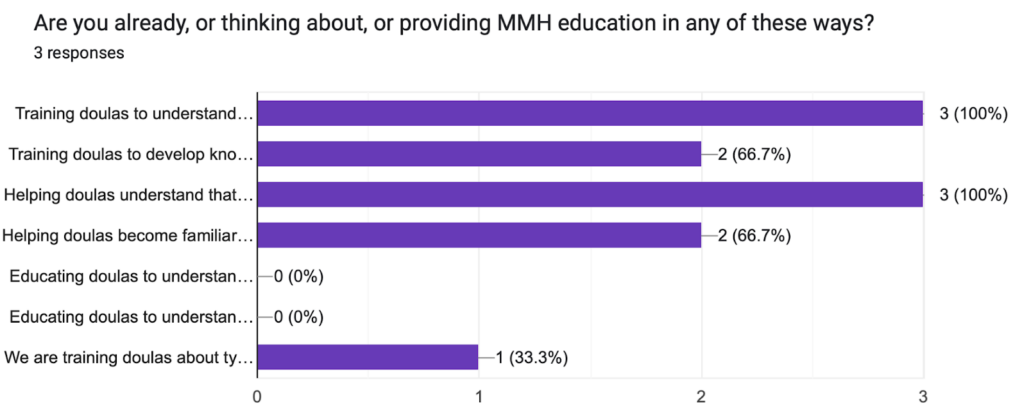
Community-Based Doula Organization Training and Services, Survey Findings
The three Community-Based Doula Organizations (CBDOs)1 whose leaders responded to our survey provided insights.
Figure 1. Community-Based Doula Organization Training
(See the questions above in the methodology section)
1. Community-Based Doula Organizations (CBDOs) are local organizations that may train doulas, connect doulas to clients, and provide other outreach (e.g., childbirth education classes). CBDOs provide care that is responsive to local contexts and culturally relevant. CBDOs may or may not have national or international training. They may often adapt national/international training to meet the unique cultural context of the community they are based in. Learn more about CBD/Os: https://pn3policy.org/pn-3-state-policy-roadmap-2023/us/community-based-doulas/
Regarding educating doulas, one said their education is offered in a variety of formats and includes “types of MMH disorders: Depression, anxiety, OCD, psychosis; Basic distinguishing factors between the common baby blues and depression; What constitutes an emergency around MMH (threatening or discussing harming self or baby).”
Another shared that they focus on MMH in all components of their training, in addition to a focused module specifically on MMH: “I’ve developed Best Practice Guides on MMH, and WisdomWay Institute Postpartum Doula/First Year Specialist Certification has a module specifically on MMH, but MMH is also woven into all other modules (i.e. Lactation, Cultural Competencies, Newborn Wellbeing and Behaviors).” This CBDO described that training staff on screening was outside the scope of what doulas should be trained to do. This CBDO also considered supporting the mental well-being of doulas: “[Trainings] support the doula to practice co-regulation as they encounter MMH challenges, to stay in the right relationship and scope of practice, to practice trauma-informed strategies and to buffer against burnout.”
The CBDOs further described training to include the divisions between their work as doulas and the healthcare system when it comes to maternal mental health. For example, one shared that they hire social workers and clinical psychologists to address mental health: “We currently partner with an organization that staffs therapists specializing in perinatal mental health and have developed a warm hand-off system between our community doulas and this organization. We also have on staff a social worker and clinical psychologist who provide mentorship support and resourcing surrounding perinatal mental health including screening tools, local support groups, local providers, strategies for recognizing and addressing signs of mental distress in their clients.”
Study Limitations
It is possible that we were not able to access all training materials for each of the national/international training and certifying bodies as some materials were not available on public websites. However, no international/national certifying organization thoroughly described the integration of MMH in training content on any publicly available resource nor on websites or external sources. Regardless, additional access and a more thorough review may have revealed further content on maternal mental health for some training/certifying organizations. Further, the three organizations that responded to the community-based doula organization (CBDOs) survey, were likely to have responded because they are proud of the maternal mental health training they provide, and that the training provided may not be universal to all CBDOs.
Regarding the doula survey, we asked doulas what, if any, maternal mental health services they provided but did not ask them whether and where they received training in maternal mental health. Therefore, it was not clear where doulas received their education about these disorders and the information they shared with clients. Further, respondents felt it was within their role to educate their clients on the risks, warning signs, and types of maternal health disorders; however, we did not assess their competency with this information.
This study did not address how doulas provide emotional support to their clients, though prior research indicates that women who received doula care had lower odds of postpartum depression or anxiety.17 Regardless of this study’s limitation regarding inquiring about emotional support, doulas may benefit from additional training on emotional regulation skills such as behavioral activation, which is currently not covered in a substantive way within doula training.8 Future research could also assess the maternal mental health content—and the sources of such content—that doulas provide to clients.
Recommendations
Core Competency Alignment and Training
- Update the Maternal Mental Health Competencies for Doulas
The core competencies should be updated by the Policy Center for Maternal Mental Health to remove references to doulas administering screening. Informed by the results from the training review and the survey results with doulas, the following two competencies are not relevant to doulas:
- Understand where to locate these screening tools and how to select and use them
- Understand the recommended frequency of screening during pregnancy and postpartum and suggested ‘cutoff’ scores to identify who may have potential anxiety or depression
Therefore the core competencies should read:
- Understand signs and symptoms of the range of MMH disorders and which factors place a woman at high risk
- Develop knowledge about valid screening tools for depression and anxiety
- Be familiar with the different types of healthcare workers involved in addressing MMH
- Understand that trouble breastfeeding can be a risk factor for anxiety and depression, and some agents used to help increase breast milk supply may trigger anxiety
- Align Training and Certification with the Core Competencies
Our results highlight opportunities for training/certification organizations to improve doula training and continuing education to equip doulas to respond to maternal mental health within their scope of practice. The updated core competencies should be integrated into training to ensure that trainees understand not just depression and anxiety, but the range of perinatal mental health conditions, their symptoms, and when to refer.
- CBDOs and certifying organizations should also consider the mental health of doulas and work proactively to prevent burnout and vicarious trauma and improve access to peer doula support and individual self-regulation skills.
Policy Recommendations
Federal or state governments should consider providing training scholarships to doulas or grants to training organizations to support doulas in obtaining additional training and continuing education in maternal mental health. This support could enable doulas to access programs such as the Policy Center for Maternal Mental Health and POEM’s maternal mental health add-on training for certified community health workers, peer support specialists, and doulas or training for health care professionals as identified by and provided by Postpartum Support International. States should ensure the current doula workforce is up-to-date with best practices in providing maternal mental health support.
References
- California Maternal Mental Health Task Force. (2017). A Report from the California Task Force on the Status of Maternal Mental Health Care. https://policycentermmh.org/california-maternal-mental-health-task-force/ ↩︎
- Horan, H. L. (2024). Doula Support as a Health Equity Strategy: Carving the Path Forward. American Journal of Public Health, 114(11), 1161–1163. https://doi.org/10.2105/AJPH.2024.307858 ↩︎
- Quiray, J., Richards, E., Navarro-Aguirre, Y., Glazer, D., Adachi, J., Trujillo, E., Perera, D., Garcia, E. P., & Bhat, A. (2024). The role of doulas in supporting perinatal mental health – a qualitative study. Frontiers in Psychiatry, 15, 1272513. https://doi.org/10.3389/fpsyt.2024.1272513 ↩︎
- March of Dimes. (n.d.). The Role of Postpartum Doulas in Mental Health Support [Blog]. Retrieved March 9, 2025, from https://www.marchofdimes.org/find-support/blog/role-postpartum-doulas-mental-health-support ↩︎
- Prenatal-to-3 Policy Impact Center. (n.d.). Community-Based Doulas—Prenatal-to-3 Policy Impact Center. Retrieved March 9, 2025, from https://pn3policy.org/pn-3-state-policy-roadmap-2023/us/community-based-doulas/ ↩︎
- Policy Center for Maternal Mental Health. (n.d.). Maternal Mental Health Screening Recommendations and Detection. Policy Center for Maternal Mental Health – Formerly 2020 Mom. https://www.2020mom.org/screening-overview ↩︎
- Salamon, M. (2023, November 22). What does a birth doula do? Harvard Health. https://www.health.harvard.edu/blog/what-does-a-birth-doula-do-202311222995 ↩︎
- Hall, E. M., Forman, S., Ostfeld, B. M., & Shahidullah, J. D. (2025). Doula support for perinatal mental health needs: Perspectives on training and practice. Midwifery, 141, 104275. https://doi.org/10.1016/j.midw.2024.104275 ↩︎
- Columbia University Mailman School of Public Health. (2016, August 3). Content Analysis Method and Examples | Columbia Public Health. https://www.publichealth.columbia.edu/research/population-health-methods/content-analysis ↩︎
- OpenAI. (2023). ChatGPT (Mar 14 version) [Large language model]. [Computer software]. https://chat.openai.com/chat ↩︎
- Policy Center for Maternal Mental Health. (n.d.). Maternal Mental Health Core Competencies. Policy Center for Maternal Mental Health. Retrieved March 9, 2025, from https://policycentermmh.org/core-competencies/ ↩︎
- Dona International. (n.d.). Continuing Education for Doulas. DONA International. Retrieved March 14, 2025, from https://www.dona.org/continuing-education/approved-continuing-ed/ ↩︎
- Childbirth International. (n.d.). Birth Doula. Childbirth International. Retrieved March 14, 2025, from https://childbirthinternational.com/birth-doula/ ↩︎
- International Childbirth Education Association. (n.d.). ICEA Certification. International Childbirth Education Association. Retrieved March 14, 2025, from https://icea.org/get-certified/ ↩︎
- Birth Arts International. (n.d.). Postpartum Doula Certification. Birth Arts International. Retrieved March 14, 2025, from https://www.birtharts.com/postpartum-doula-certification/ ↩︎
- Childbirth and Postpartum Professional Association. (n.d.). Training & Certification. CAPPA. Retrieved March 14, 2025, from https://cappa.net/training-certification/ ↩︎
- Falconi, A. M., Bromfield, S. G., Tang, T., Malloy, D., Blanco, D., Disciglio, R. S., & Chi, R. W. (2022). Doula care across the maternity care continuum and impact on maternal health: Evaluation of doula programs across three states using propensity score matching. eClinicalMedicine, 50, 101531. https://doi.org/10.1016/j.eclinm.2022.101531
↩︎
For a comprehensive update on state doula Medicaid implementation efforts, view this resource from the National Health Law Program.To review the Policy Center’s Core competencies, view this resource: policycentermmh.org/lay-professionals/
Contributors:
Report Writing: Regan Moss, Policy Center
Conceptualization, Topic Supervision, Policy Writing: Joy Burkhard, Policy Center
Subject Matter Review: Twylla Dillion Health Connect One
Copy Editors: Kelly Nielson, Cindy Herrick, Joy Burkhard, & Kate Rope, Policy Center