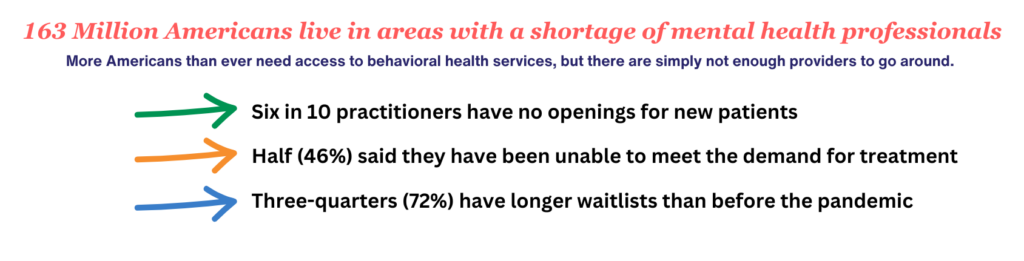
America’s mental and behavioral health care system is under-resourced, fragmented, and confusing. Today, more Americans have health insurance than ever before, but having coverage does not guarantee access to care, particularly when it comes to behavioral health services
Coverage for behavioral health may be separate – or “carved out” – from coverage for physical health

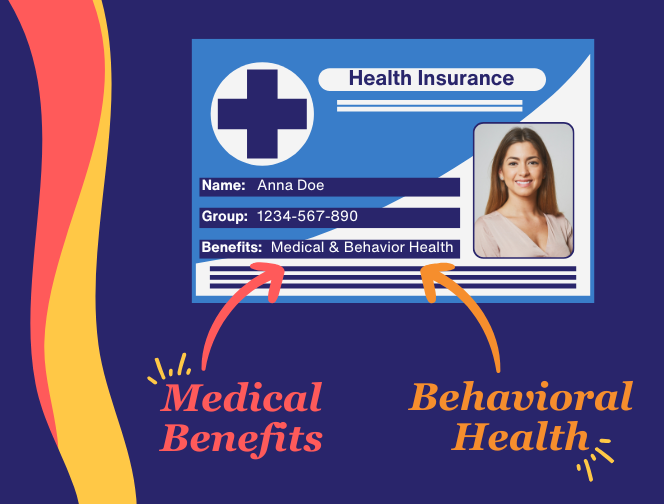
More often than not, specialty insurance companies administer behavioral health benefits. This can result in an individual or family having one health insurance card but two different phone numbers for member services, provider networks, referral systems, and authorization policies.
This bifurcation of behavioral health benefits from medical benefits creates barriers to care for people who already feel overwhelmed, are struggling to cope, and/or are reluctant to seek help. Likewise, it causes unnecessary confusion and administrative burden for providers trying to meet the whole-person needs of their patients.
MENTAL HEALTH
includes our emotional, psychological, and social well-being. It affects how we think, feel, and act, and helps determine how we handle stress, relate to others, and make choices. See SAMHSA: https://www.samhsa.gov/mental-health.
BEHAVIORAL HEALTH
generally refers to mental health and substance use disorders, life stressors, crises, and stress-related physical symptoms. Behavioral health care refers to the prevention, diagnosis, and treatment of those conditions.
Behavioral Health Integration is Key to Addressing Provider Shortages, Improving Outcomes
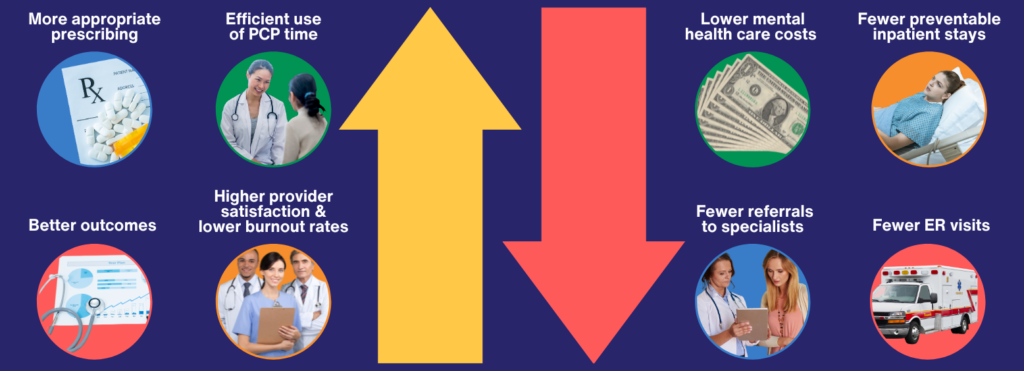
Behavioral health integration (BHI) makes it easier for primary care and obstetrical providers to include mental and behavioral health screening, treatment, and specialty care into their practices. It is a team-based approach that emphasizes collaboration among providers and addresses a patient’s needs holistically.
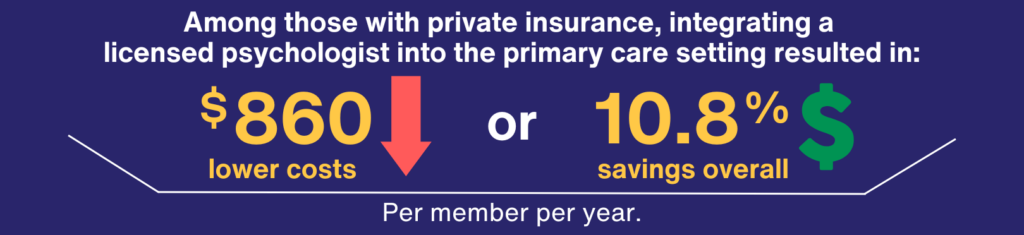
Multiple studies demonstrate how BHI improves outcomes, lowers costs, and increases patient and provider satisfaction. A recent randomized controlled trial showed patients who received depression care in a primary care setting that had integrated behavioral health clinicians had better outcomes than those who received usual care, including greater use of coping strategies more often, adherence to medications, and patient satisfaction.
Health Insurers Should Integrate Behavioral Health Benefits, Networks, and Contracts
Many patients with mild or temporary behavioral health needs could be treated within the primary (or obstetrical) care setting. However, primary and obstetrical care providers who want to offer more behavioral services in their practices often cannot because those benefits are carved out of their contracts. They are forced to refer patients to mental health providers through specialty insurance plans, which exacerbates shortages and delays access to care for those with more severe and/or ongoing needs.
Providers should be able to contract for all appropriate services through major medical insurers rather than having to contract separately for BH services with subcontracted benefit administrators.
“We don’t carve out heart care, so why do we carve out mental health care?”
– Joy Burkhard,
Founder/CEO, Policy Center for Maternal Mental Health
In Summary
We have made significant strides in expanding health insurance to 92 percent of the population and ensuring mental and behavioral health is covered at parity with physical health care. But there is much work that remains to translate coverage for mental health services into access to mental health care.
We must kill the carveout of mental health services to separate insurance companies and instead fully integrate services, networks, and contracts. This will reduce confusion, streamline administrative processes, and promote higher quality care at lower cost.